Perinatal Hospice and Neonatal Palliative Care
December 12, 2017
|
Prof. G. Noia
Originally presented at the 2017 MaterCare Rome Conference
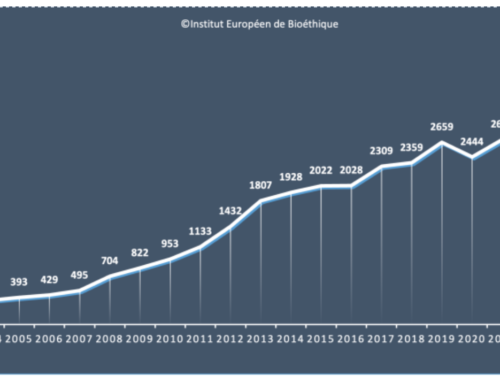
The prenatal panorama of the last 40 years has shown lights and shadows in the defence of the nascent life and in the custody of a value whose preciousness should be transversal to every ideology and to any difference in anthropological evaluation. “This essential invisible to the eyes” should be the primary objective of every human aggregation such as photosynthesis which, although not visible, is recognized as the primary source of universal energy. In Italy, if on the one hand we have recorded a eugenistic attitude towards fragile life and burdened with malformations (the rate of eugenic voluntary abortion after the 12 weeks i.e. after the third month, it moved from 0.5% in 1981 to 5% in 2015), in the same years we have spread and developed the concept of fetal medicine, that is, the possibility of treating the child in utero even in conditions of severe pathologies (Noia G. et al. “Terapie fetali invasive”-Editrice Universo – Rome, 1998; Noia G. et al. “Terapie fetali”-Poletto Editore – Vermezzo-MI, November 2009).
At the Policlinico Gemelli already in the years ‘ 80 a synergy between gynecological, neonatologists and other medical figures such as infantile neurosurgeons, cardiologists pediatricians and pediatric surgeons, has carried on the idea that the fetus was a patient in all respects. Interdisciplinary meetings were organised to optimise prenatal therapies and interventions, and specific perinatal interventions for all types of fetal diseases.
Throughout the world, ultrasonografic techniques have become a basic element to drive invasive approaches to a fetal compartment and to make a series of diagnostic and therapeutical acts aimed at treating the fetus as a patient in all respects, with a fair ethical and scientific assessment of risk-benefit. This is the fetal therapy.
In our Center the intravascular approach (fetal blood sampling from the umbilical cord in case of fetal anemia and correction of the same via the same pathway with fetal transfusions), has resulted in survival from 40 to 92%. In 32 cases fetal curarization were performed to block the extreme mobility of the fetus and allow transfusion. Intramniotic approaches such as amnioinfusion (placing saline solution in the amniotic cavity after membrane rupture) improved survival from 0 to 50% while drainage and aspirations of large fetal ovarian cysts (about 4 cm.), prevented the torsion and loss of the ovary in 30 cases of girls who were born with intact ovaries and preserved. Also the intraurinary approach with aspirations and drainage from the pielic cavity or bladder, they improved survival from 20 to 65% and in cases of non-immunological fetal hydrops (severe condition whereby the fetus shows presence of fluids in the thorax and abdomen as an expression of hemodynamic decompensation), integrated and multiple treatments have resulted in survival from 12 to 48% and long-distance follow-up shows an excellent outcome in 79% of children born. These are just a few examples belonging to a case study of about 8000 procedures carried out in the last 30 years in our center.
Alongside these invasive procedures, the fetal palliation was also developed, i.e. that set of procedures aimed at accompanying invasive interventions that crossed the fetal body, to avoid the pain of the fetus. This treatment aimed to make a analgesia (nociceptive palliation), but the whole of these therapeutical attitudes also aimed to extend the peritoneal and pleural membranes in order to avoid the distension of the same, very rich in nerve endings and therefore to avoid chronic suffering from distension (clinical palliation). Whereas the perception of pain on the part of the fetus starts already from the 18th week and that the ability to manage pain (pain modification system) is completed at the 27th week, it is very well understood the importance of these palliative, analgesic and/or clinical treatments, to limit the damage that the perception of pain by the fetus can create to the anatomic and neuro physiological development of the central nervous system of the future child.
The results obtained in the Diagnosis and Fetal Therapy Center of the Policlinico Gemelli, by implementing the so-called integrated fetal therapy, they show that even in serious fetus-neonatal pathologies, or conditions of terminality or life limiting, there are possibilities of intervention to rescue gestational capacity to all those families burdened by an unfortunate diagnosis.
The third aspect, which is consequential to this culture of prenatal but which is clear the therapeutic evolution, is the aspect of accompaniment and all this is called Perinatal Hospice which is not only a place in a medical environment, with medical interventions done by doctors with experience in this field, but also a way of shared medicine, in which even families play a role of support (Noia G. et al. “Il Figlio Terminale”-Nova Millennium Romae – Rome, February 2007; Noia G. et al. “La terapia dell’accoglienza”-If press – Moro-FR, December 2010). In the international literature we know that infant mortality within the first year recognizes in malformations the first cause of mortality (1.2 per thousand-National Vital Statistics reports, 2011 – CDC – USA).
In recent years several authors (Calhoun BC et al. J Reprod Med. 2003; 48 (5): 343-8 – d ‘ Almeida M et al. Journal of American physician and surgeons. 2006; 11 (2): 52-55 – Breeze AC et al. Arch Dis Child Fetal newborn ed. 2007; 92 (1): f56-8 – Leuthner s et al. Fetal concerns program. MCN am J Maternal Child Nursing. 2007; 32 (5): 272-8) have studied the problem of life limiting conditions in a frontal way, bringing several case of eligible conditions as life limiting pathologies.
In the experience reported, the percentages of continuation of the pregnancy ranged from 37% to 87%. In the 25 years of accompanying the weak life, in our center we identified 432 cases eligible for life limiting conditions from 1990 to 2015, checking acceptance to continue pregnancy in 94% of cases.
The perception of the importance of care for life limiting conditions is growing increasingly, as reported by Ortigoza Escobar et al. Global Congress of maternal and Infant health, 2010. On 116 doctors specialists in obstetrics and gynecology and in 6 hospitals of the 3rd level in Barcelona, grew from 31.9% to 52.6%.
In conclusion, the Perinatal Hospice has a cultural impact between two anthropologically opposed ways of thinking: the first lives of the illusion that eliminating suffering fetus we can eliminate suffering, the second instead in the most total respect of the preciousness of human life, without looking at the dimensions of the human being but only to its value, seeks to prevent diseases, seeks to heal them, seeks to limit the physical and psychological damage of the sick and families , seeks to soothe the physical and psychological suffering, strong of the assumption of three methodologies to deal with human suffering: Prevent, cure, relief (Prevent, cure, soothe pain). But all this expresses the concept of human solidarity, of shared medicine, and it translates into a single expression: I care (I take care of you).
-Professor G. Noia