Vaccine Science Diplomacy and “The Phenomenon of Man”
Peter Hotez, MD, PhD, FAAP, FASTMHhttps://orcid.org/0000-0001-8770-1042View all authors and affiliationsOnlineFirsthttps://doi.org/10.1177/00243639241245105
- Contents
- PDF / ePub
Abstract
The central tenets of international scientific collaborations leading to the development, testing, and the equitable distribution vaccines to combat poliomyelitis, smallpox, COVID-19, and other devasting infections, first accelerated in the mid-twentieth century. The genesis of vaccine science diplomacy also coincides with the publication of Le Phénomène Humain (The Phenomenon of Man) shortly after the death of its author, the French Jesuit priest and scientist, Dr. Teilhard de Jardin. Several tenets of Teilhard’s posthumous essay, including our collective consciousness, and the “conjugated faces” of science and religion, are relevant to a modern vaccine diplomacy framework, even if Teilhard may not have specifically addressed vaccines in his writings. This could also include the potential for arriving at an “omega point” through international scientific collaboration and joint vaccine development, while simultaneously avoiding the destructive forces of anti-vaccine or anti-science activism. Collaborations between the Vatican, Catholic research universities and institutions, and leaders of the Catholic-majority nations in Africa, Asia, and Latin America in an integrated framework might accelerate these activities as they apply to both pandemic threats and neglected diseases of poverty.
Introduction
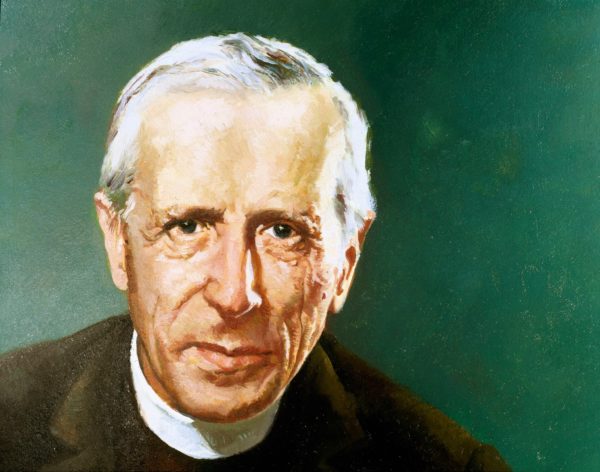
The French Jesuit priest, theologian, and scientist, Dr. Teilhard de Jardin, investigated human origins and evolution, and he lectured, and traveled widely. After obtaining his doctoral degree in science in Paris, France, he conducted extensive paleontological investigations in China, later continuing his research in East Africa and Northern India. Teilhard’s posthumously published book (in 1955), Le Phénomène Humain (The Phenomenon of Man) emphasized many aspects of the human condition and evolution in a bold effort to reconcile science and religion.In The Phenomenon of Man, Teilhard saw science and religion as mutually reinforcing or as “the two conjugated faces or phases of one and the same complete act of knowledge” (Teilhard de Chardin 2008). He eloquently stated:After close on two centuries of passionate struggles, neither science nor faith has succeeded in discrediting its adversary. On the contrary, it becomes obvious that neither can develop normally without the other. (Teilhard de Chardin 2008)Teilhard also saw the potential for human evolution to advance a mystical concept of the noosphere, or “a harmonized collectivity of consciousness equivalent to a sort of super-consciousness” (Teilhard de Chardin 2008). Should this happen he states: “Disease and hunger will be conquered by science and we will no longer need to fear them in any acute form” (Figure 1) (Teilhard de Chardin 2008). Eventually this utopia could coalesce into a singularity, which he designated as an omega point.

OPEN IN VIEWERTeilhard’s thesis was and still is considered controversial, and The Phenomenon of Man generates mixed responses in both the scientific and theological academic communities. Notably, the British evolutionary biologist and science communicator, Sir Julian Huxley, was both a contemporary and an enthusiastic colleague of Teilhard. He wrote in 1958 how Teilhard’s vision was one of “extensive interrelation and cooperation” and summarized the book as follows:We, mankind, contain the possibilities of the earth’s immense future, and can realise more and more of them on condition that we increase our knowledge and our love. That, it seems to me, is the distillation of The Phenomenon of Man. (Teilhard de Chardin 2008)The relationship between the Catholic Church and Teilhard’s writings was complex, and much of his work went unpublished in his lifetime (Grumett and Bentley 2018). More recently, Teilhard’s essay and other writings have been applied towards the bioethics of other aspects of modern biotechnology, including gene editing (Šuleková and Fitzgerald 2019).
Vaccine Science Diplomacy
Although Teilhard’s writings may not have specifically address vaccines, an example of a reconciliation between science and religion and an aspiration towards a noosphere or omega point is potentially the concept and framework of vaccine science diplomacy (Hotez 2014a). The term refers to an international collaboration for the joint development of vaccines or related technology (Hotez 2014a). This could include scientists representing nations with ideologically divergent governments. A prime example is the oral polio vaccine first developed in the laboratory of Dr. Albert Sabin based at the Cincinnati Children’s Hospital in the United States (US). The vaccine was not actually produced in large quantities and made available for widescale testing until Sabin’s oral polio strains were sent to the Soviet Union (Hotez 2014a, 2021a). This happened at the beginning of a Cold War space race. Led by Dr. Sabin’s Russian counterpart, Dr. Mikhail Chumakov, the new vaccine was tested in millions of Soviet citizens in the USSR (Hotez 2021a). Such essential studies laid the foundation for vaccine licensure and ultimately the global distribution of the oral polio vaccine now leading to disease eradication. Years later the USSR and the US, as well as the World Health Organization collaborated to scale-up production of the smallpox vaccine. Through international vaccine diplomacy, smallpox was eradicated in the late 1970s (Hotez 2014a, 2021a). The reality that two nations or even Cold War enemies could resolve their differences around common goals in science and technology, represented an important step towards Teilhard vision of harmony or coalescence: “Some sort of unanimity will reign over the entire mass of the noosphere” (Teilhard de Chardin 2008).Another important step in international science diplomacy was the creation of the US Envoy Program in 2009. The establishment was announced by then newly inaugurated President Barack Obama in a landmark speech entitled “A New Beginning.” He delivered these remarks at the University of Cairo, a historical seat of learning in the modern Arabic world (Hotez and Kassem 2016); they were intended to signal a fresh start in scientific cooperation between the US and the world’s Muslim-majority nations belonging to the Organization of the Islamic Conference (OIC). As a US Science Envoy my charge was to build vaccine science diplomacy initiatives with OIC countries in the Middle East and North Africa (Hotez 2021a). This was a precarious time because it coincided with the Islamic State of Iraq and Syria (ISIS) occupation and civil conflicts in Yemen leading to a resurgence in vaccine preventable infections such as polio and measles, as well as vector-borne illnesses such as leishmaniasis (Hotez 2015). However, that was exactly the point – creating a framework during times of strife represents a cornerstone of vaccine science diplomacy.
COVID-19 Vaccine Nationalism
Tragically, the lessons learned from Cold War vaccine science diplomacy and those from the Obama Administration’s US Science Envoy Program did not translate into global vaccine equity during the COVID-19 pandemic. This became especially apparent in the pandemic’s first two years. The US Operation Warp Speed COVID-19 vaccine program successfully accelerated new technologies (Kim et al. 2021), including mRNA, adenovirus-vector, and particle vaccines, but these vaccines could not be produced in sufficient quantities. For the first two years of the pandemic, the US and Canada, as well as the United Kingdom (UK), Israel, and Western European nations had privileged access to mRNA vaccines from Pfizer and Moderna, leaving out most of the world’s low- and middle-income countries (LMICs) (Hotez 2022a). According to one estimate, over this period roughly only one-third of people on the African continent received a dose of a COVID-19 vaccine, whereas high-income nations (representing less than 15% of the global population) purchased more than one-half of global vaccine doses (Lalani et al. 2023). In many respects this situation was both predicted and predictable given the reality that almost any new technology requires time to produce it at a scale requiring several billions of doses. For much of 2021, the first year when mRNA vaccines became widely available in high-income countries, they were mostly unavailable in LMICs.Compounding this situation were the actions of China and Russia. In the case of China, two vaccines that employed an older whole-inactivated virus vaccine technology were produced, and these were sold or bartered to LMICs and other nations in bilateral exchanges. Similarly, Russia engaged in transactional and bilateral interactions that offered an adenovirus-vectored vaccine that was named Sputnik V [9-11] (Hotez 2022a; Lalani et al. 2023; Sachs et al. 2022). These vaccines did not provide the same level of vaccine protection as the mRNA vaccines, especially against the emerging omicron variants (Cheng et al. 2022). In place of vaccine science diplomacy, both China and Russia engaged in what some referred to as vaccine nationalism (Hotez 2022a; Lalani et al. 2023; Sachs et al. 2022). Beyond the obvious humanitarian tragedy that resulted from LMICs not having access to the best or highest performing COVID-19 vaccines was the grim reality that the terrible delta variant emerged from an unvaccinated population in India in early 2021, while the omicron variants arose from and under-vaccinated population on the African continent later that year. Therefore, both North American and European countries also suffered a terrible loss of human life because of failures in global vaccine science diplomacy.
Corbevax and IndoVac
To accelerate vaccine equity and diplomacy, but also bypass toxic vaccine nationalism, efforts were made to create alternative pathways for COVID-19 vaccine production and distribution. One of the successful approaches included partnerships between US or UK academic institutions and LMIC vaccine producers to directly transfer technology for local scale-up, production, and distribution. Thus, Oxford University’s Jenner Vaccine Institute worked with AstraZeneca to transfer its adenovirus vectored vaccine technology to the Serum Institute of India (Pune, India) leading to the production of Covishield (Hotez 2023d; Sachs et al. 2022). However, the Texas Children’s Hospital Center for Vaccine Development (Texas Children’s CVD) took this one step further by bypassing multinational pharmaceutical companies altogether and directly transferring its prototype vaccine technology directly to LMIC producers in India and Indonesia (Hotez et al. 2023). This approach was considered more aligned with the original framework for vaccine diplomacy since it involved direct and international cooperation between scientists and was done in ways to maximize access without seeking large financial returns.The Texas Children’s CVD is an academic non-profit product development partnership that develops low-cost recombinant protein vaccines for schistosomiasis, hookworm infection, Chagas disease, and leishmaniasis. Each is a vaccine for a parasitic disease primarily affecting LMICs. They are sometimes known as “antipoverty vaccines” because the diseases they target trap people in poverty due to their disabling effects on worker productivity or child development and women’s reproductive health (Hotez et al. 2016). Beginning in the 2010s, coronavirus vaccines for severe acute respiratory syndrome (SARS) and Middle Eastern respiratory syndrome (MERS) also became incorporated into the Texas Children’s CVD vaccine portfolio (Chen et al. 2017, 2020; Nyon et al. 2018), mostly because these vaccines, like parasitic disease vaccines, were orphaned by the multinational pharma companies. When the COVID-19 virus (SARS-2) virus sequence became available in January 2020, the Texas Children’s CVD worked to flip its coronavirus vaccine towards this pathogen, ultimately producing a low-cost and patent-free COVID-19 vaccine for global health. The Texas Children’s CVD COVID-19 vaccine technology utilizes genetic engineering in yeast followed by microbial fermentation to produce a recombinant protein version of the COVID-19 spike protein receptor binding domain (Hotez et al. 2023; Hotez and Bottazzi 2022). This is a technology similar to that used to produce the yeast-derived recombinant hepatitis B vaccine, one of the most widely used vaccines for children with an outstanding safety track-record. It can also be produced at extremely low-cost and is generally stable at simple refrigeration temperatures, without the need for onerous freezing requirements. In the case of the Texas Chlidren’s CVD vaccine technology, it is formulated on aluminum particles (alhydrogel) together with an oligonucleotide toll-like receptor 4 immunostimulant as an adjuvant (Chen et al. 2021, 2022; Hotez et al. 2023; Hotez and Bottazzi 2022; Pino et al. 2021; Pollet et al. 2021, 2022).The Texas Children’s CVD COVID-19 vaccine technology was licensed to two vaccine manufacturers located in India (Biological E) and Indonesia (BioFarma), respectively.In India, Biological E produced several hundred million doses of vaccine that utilized the Texas Children’s CVD antigen technology. The vaccine, known as CORBEVAX became one of the first entirely Indian produced and owned COVID-19 vaccines (Jaggaiahgari et al. 2022; Thuluva et al. 2022a; Thuluva et al., 2022b). CORBEVAX underwent clinical trials in India (phase 1–3) and it was authorized in the last quarter of 2022 following an extensive clinical superiority study that compared it to Covishield. Approximately 74 million doses of CORBEVAX have been administered as a primary immunization and booster to school children, with 10 million adults receiving CORBEVAX as a booster after previously receiving either Covishield or Covaxin (whole-inactivated virus vaccine made by Bharat Biotech in India). These doses were delivered at around $3 dollars per dose. The experience so far is that the vaccine has exhibited an excellent safety profile, and parents largely supported its use for pediatric immunizations in India. This feature, together with its low-cost and likely durable protection because virus neutralizing antibodies to the vaccine do not decline rapidly, made CORBEVAX an attractive vaccine for resource-poor settings. The bottom line was that CORBEVAX checked mulitple boxes for a global health vaccine.In Indonesia, a major vaccine manufacturer known as BioFarma also produced a closely related Texas Children’s CVD vaccine technology resulting in the authorization and distribution of INDOVAC. In addition, because the Texas Children’s CVD COVID-19 vaccine technology is vegan, the Indonesian Government and BioFarma successfully partnered with the clergy and Muslim community to achieve Halal certification for INDOVAC.In each of these cases, vaccine diplomacy prevailed because of concerted efforts between US or UK academic scientists and LMIC vaccine producers. They also emphasize that multinational pharma companies do not necessarily have to lead global health vaccine initiatives. Instead, these examples provide some proof-of-concept that it is possible to approach Teilhard’s concept of the omega point without the reliance on “big pharma.” It is possible to create parallel paths. The Texas Children’s CVD is currently preparing an XBB booster of their COVID-19 vaccine technology rapidly progressing through clinical trials in India (Hotez 2023c), with downstream plans and aspirations to develop additional vaccines to prevent future pandemics or endemic neglected tropical diseases.
Overcoming Vaccine Hesitancy
Promoting equity through vaccine science diplomacy is an essential element for ensuring global access, but it faces an accelerating threat because of rising hesitancy and vaccine refusal. An essential point that is not always intuitively obvious: Today, overcoming vaccine hesitancy and refusal is as fundamental to achieving vaccine equity as promoting vaccine diplomacy (Hotez 2023d). The reason for this tragic reality is based on the extraordinary acceleration of vaccine refusal that began in the years immediately preceding the COVID-19 pandemic.Resistance to vaccines and vaccinations is as old as the first immunizations going back to variolation for smallpox in the founding British colonies of North America (Hotez 2018). However, the modern era of hesitancy began in the early 2000s after false accusations arose that claimed vaccines cause autism or neurodevelopmental disorders. An antivaccine movement ignited in the UK, but it amplified in the US where it reduced childhood immunization rates (Hotez 2018; Hotez et al. 2020; Lo and Hotez 2017). By the year 2019, the World Health Organization declared vaccine hesitancy a leading global health threat (Hotez et al. 2020). In the US, the antivaccine movement became especially pernicious because it acquired a political dimension, especially in conservative US states where libertarian concepts of “health freedom” or “medical freedom” prevailed (Hotez 2021b, 2023a, 2023b). This meant that the antivaccine movement transitioned from a grassroots campaign into one that was organized, adequately financed, and driven by a unique brand of American politics (Carpiano et al. 2023).Antivaccine activism is a new reality that extends beyond the borders of the US to become a dangerous globalizing force (Hotez 2022b). Specifically, US style of antivaccine activities have become pervasive as they extend into Canada and Europe (Hotez 2023a). Now this is expanding into LMICs, including Brazil (Daniels 2021), and several African nations (Hotez 2022b, 2023a). Antivaccine and anti-science activism or aggression is a relatively new and destructive aspect of modern society, but one that is growing quickly so that it will haunt us for the foreseeable future. For all these reasons, countering vaccine refusal and hesitancy has become an essential element of effective vaccine diplomacy (Hotez 2023d).
Concluding Remarks
The universe of anti-science is expanding rapidly and threatens the enormous global health gains of the last two decades, including the accelerated progress in vaccine development that occurred for COVID-19 vaccines. Vaccine nationalism demonstrated the fragility of vaccine diplomacy and equity, but now anti-science is positioned to cause further unraveling. Teilhard saw the potential of science to achieve harmonization and fight disease, but he also recognized how “evil may go on growing alongside good, and it too may attain its paroxysm at the end in some specifically new form” (Teilhard de Chardin 2008). Therefore, we must recognize the real threat of antivaccine and anti-science activism as it globalizes and potentially threatens our entire vaccine ecosystem and universal health coverage for both pediatric and adult immunizations. As the World Health Organization embarks on a new Immunization Agenda 2030, including what they refer to as “the big catch-up” to restore consistency to global immunization campaigns (World Health Organization 2023), we should be mindful of the warnings of Teilhard. At the same time, he offers us a framework for promoting vaccine diplomacy and equity between nations. This might be fertile ground for future explorations in religious philosophy, and for examining the life and works of Teilhard, in particular.Teilhard’s vision for reconciling science and religion still has relevance in this modern age of vaccines. A new framework for vaccine science diplomacy will require parallel pathways of promoting vaccine development and distribution through both the multinational pharma companies and the LMIC vaccine producers in collaboration with academic product development partnerships. Such vaccine diplomacy efforts could apply to both new vaccines for pandemic threats and widespread neglected diseases such as HIV/AIDS, malaria, tuberculosis, and the neglected tropical diseases such as hookworm infection, schistosomiasis, leishmaniasis, and Chagas disease. Such illnesses are widespread in LMICs, including many Catholic- or Christian-majority nations, such as Angola, Democratic Republic of the Congo, and Uganda on the African Continent, Philippines in Southeast Asia, and of course most of the Latin American nations (Hotez 2011; Hotez 2014b). The diseases constitute the most common afflictions of people who live in poverty in these countries.Given the special emphasis that Pope Francis has placed on helping the world’s poor, together with his frequent visits to African, Asian, and Latin American countries, it would stand to reason that vaccine diplomacy could be incorporated in such outreach efforts. Pope Francis has been an enthusiastic supporter of COVID immunizations, but in addition in 2016, The Pontifical Council for Health Care Workers hosted a historic summit and international conference at the Vatican on neglected diseases. The summit was entitled “Towards a Culture of Health that is Welcoming and Supportive at the Service of People with Rare and Neglected Pathologies,” which I participated in and where we discussed in depth the opportunities for international cooperation to develop new vaccines for these conditions (Hotez 2016). Therefore, there are opportunities for the Vatican, the Catholic Church, and the major Catholic research universities, together with health ministers or leaders in the disease-affected Catholic-majority nations to also embrace a larger vision of vaccine diplomacy. Potentially this could be initiated through the Pontifical Council for Health Care Workers, the Pontifical Academy of Sciences or other mechanisms to be determined. Launching such an initiative will also require an equally robust effort to counter vaccine nationalism and a new level of antivaccine aggression and activism. We are living in a precarious time when global health is under threat.
Declaration of Conflicting Interests
The team of scientists at Texas Children’s Hospital Center for Vaccine Development including its co-director Professor Peter Hotez are co-inventors on non-revenue generating patents for neglected tropical diseases owned by Baylor College of Medicine (BCM). They are also co-inventors of a COVID-19 recombinant protein vaccine technology owned by BCM that was recently licensed by Baylor Ventures non-exclusively and with no patent restrictions to several companies committed to advance vaccines for low- and middle-income countries. These include Biological E (India), BioFarma (Indonesia), Incepta (Bangladesh) and ImmunityBio (United States with partnerships is the African Continent including Botswana and South Africa). The co-inventors have no involvement in license negotiations conducted by BCM. Similar to other research universities, a long-standing BCM policy provides its faculty and staff, who make discoveries and that result in a commercial license, a share of any royalty income. Any such distribution will be undertaken in accordance with BCM policy. In addition, Dr. Hotez is also the author of several books published by academic presses (ASM-Wiley) and Johns Hopkins University Press, and he receives modest royalty income from this activity.
Funding
The author received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Peter Hotez https://orcid.org/0000-0001-8770-1042
References
Carpiano R. M., Callaghan T., DiResta R., Brewer N. T., Clinton C., Galvani A. P., Lakshmanan R., W. E.et al. 2023. “Confronting the Evolution and Expansion of Anti-Vaccine Activism in the USA in the COVID-19 era.” Lancet (London, England) 401 (10380): 967–970. https://doi.org/10.1016/S0140-6736(23)00136-8.GO TO REFERENCEPubMedGoogle ScholarChen W. H., Chag S. M., Poongavanam M. V., Biter A. B., Ewere E. A., Rezende W., Seid C. A., E. M.et al. 2017. “Optimization of the Production Process and Characterization of the Yeast-Expressed SARS-CoV Recombinant Receptor-Binding Domain (RBD219-N1), a SARS Vaccine Candidate.” Journal of Pharmaceutical Sciences 106 (8): 1961–1970. https://doi.org/10.1016/J.XPHS.2017.04.037.GO TO REFERENCEPubMedGoogle ScholarChen W. H., Pollet J., Strych U., Lee J., Liu Z., Kundu R. T., Versteeg L., M. J.et al. 2022. “Yeast-expressed Recombinant SARS-CoV-2 Receptor Binding Domain RBD203-N1 as a COVID-19 Protein Vaccine Candidate.” Protein Expression and Purification 190: 106003. https://doi.org/10.1016/J.PEP.2021.106003.GO TO REFERENCEPubMedGoogle ScholarChen W. H., Tao X., Agrawal A. S., Algaissi A., Peng B. H., Pollet J., Strych U., M. E.et al. 2020. “Yeast-expressed SARS-CoV Recombinant Receptor-Binding Domain (RBD219-N1) Formulated with Aluminum Hydroxide Induces Protective Immunity and Reduces Immune Enhancement.” Vaccine 38 (47): 7533–7541. https://doi.org/10.1016/J.VACCINE.2020.09.061.GO TO REFERENCEPubMedGoogle ScholarChen W. H., Wei J., Kundu R. T., Adhikari R., Liu Z., Lee J., Versteeg L., C.et al. 2021. “Genetic Modification to Design a Stable Yeast-Expressed Recombinant SARS-CoV-2 Receptor Binding Domain as a COVID-19 Vaccine Candidate.” Biochimica et Biophysica Acta (BBA) – General Subjects 1865 (6): 129893. https://doi.org/10.1016/J.BBAGEN.2021.129893.GO TO REFERENCEPubMedGoogle ScholarCheng S. S., Mok C. K., Li J. K., Ng S. S., Lam B. H., Jeevan T., Kandeil A., A.et al. 2022. “Plaque-neutralizing Antibody to BA.2.12.1, BA.4 and BA.5 in Individuals with Three Doses of BioNTech or CoronaVac Vaccines, Natural Infection and Breakthrough Infection.” Journal of Clinical Virology 156: 105273. https://doi.org/10.1016/J.JCV.2022.105273.GO TO REFERENCEPubMedGoogle ScholarDaniels J. P. 2021. “Health Experts Slam Bolsonaro’s Vaccine Comments.” Lancet (London, England) 397 (10272): 361. https://doi.org/10.1016/S0140-6736(21)00181-1.GO TO REFERENCEPubMedGoogle ScholarGrumett D., Bentley P. 2018. “Teilhard de Chardin, Original sin, and the six Propositions.” Zygon® 53 (2): 303–330. https://doi.org/10.1111/ZYGO.12398.GO TO REFERENCEGoogle ScholarHotez P. J. 2011. “Neglected Tropical Diseases in the Catholic World.” PLOS Neglected Tropical Diseases 5 (4): e1132. https://doi.org/10.1371/journal.pntd.0001132.GO TO REFERENCEGoogle ScholarHotez P. J. 2014a. “Vaccine Diplomacy”: Historical Perspectives and Future Directions.” PLOS Neglected Tropical Diseases 8 (6): e2808. https://doi.org/10.1371/JOURNAL.PNTD.0002808.Google ScholarHotez P. J. 2014b. “Global Christianity and the Control of its Neglected Tropical Diseases.” PLOS Neglected Tropical Diseases 8 (11): e3135. https://doi.org/10.1371/journal.pntd.0003135.GO TO REFERENCEGoogle ScholarHotez P. J. 2015. “Vaccine Science Diplomacy: Expanding Capacity to Prevent Emerging and Neglected Tropical Diseases Arising from Islamic State (IS)–Held Territories.” PLOS Neglected Tropical Diseases 9 (9): e0003852. https://doi.org/10.1371/JOURNAL.PNTD.0003852.GO TO REFERENCEGoogle ScholarHotez P. J. 2016. “The Vatican Takes on Neglected and Rare Diseases.” Baylor College of Medicine Momentum (Blog), December 5, 2016. https://blogs.bcm.edu/2016/12/05/the-vatican-takes-on-neglected-and-rare-diseases/GO TO REFERENCEGoogle ScholarHotez P. J. 2018. Vaccines did not Cause Rachel’s Autism : My Journey as a Vaccine Scientist, Pediatrician, and Autism Dad. Baltimore.: Johns Hopkins University Press.Google ScholarHotez P. J. 2021a. “Preventing the Next Pandemic.” In Preventing the Next Pandemic. Baltimore: Johns Hopkins University Press, 208. https://doi.org/10.56021/9781421440392.Google ScholarHotez P. J. 2021b. “America’s Deadly Flirtation with Antiscience and the Medical Freedom Movement.” The Journal of Clinical Investigation 131 (7), https://doi.org/10.1172/JCI149072.GO TO REFERENCEPubMedGoogle ScholarHotez P. J. 2022a. “COVID-19 Vaccines: the Imperfect Instruments of Vaccine Diplomacy.” Journal of Travel Medicine 29 (8), https://doi.org/10.1093/JTM/TAAC063.PubMedGoogle ScholarHotez P. J. 2022b. “Will Anti-Vaccine Activism in the USA Reverse Global Goals?” Nature Reviews Immunology 22 (9): 525–526. https://doi.org/10.1038/s41577-022-00770-9.PubMedGoogle ScholarHotez P. J. 2023a. Deadly Rise of Antiscience: A Scientist’s Warning. Baltimore: Johns Hopkins University Press, 240.Google ScholarHotez P. J. 2023b. “Global Vaccinations: New Urgency to Surmount a Triple Threat of Illness, Antiscience, and Anti-Semitism.” Rambam Maimonides Medical Journal 14 (1): e0003. https://doi.org/10.5041/RMMJ.10491.GO TO REFERENCEGoogle ScholarHotez P. J. 2023c. “SARS-CoV-2 Variants Offer a Second Chance to fix Vaccine Inequities.” Nature Reviews. Microbiology 21 (3): 127–128. https://doi.org/10.1038/S41579-022-00824-8.GO TO REFERENCEPubMedGoogle ScholarHotez P. J. 2023d. “Global Vaccine Access Demands Combating Both Hesitancy and Inequity.” Health Affairs. 42 (12): 1681–1688.CrossrefGoogle ScholarHotez P. J., Adhikari R., Chen W.-H., Chen Y.-L., Gillespie P., Islam N. Y., Keegan B., R.et al. 2023. “From Concept to Delivery: A Yeast-Expressed Recombinant Protein-Based COVID-19 Vaccine Technology Suitable for Global Access.” Expert Review of Vaccines 22 (1): 495–500. https://doi.org/10.1080/14760584.2023.2217917.PubMedGoogle ScholarHotez P. J., Bottazzi M. E. 2022. “Whole Inactivated Virus and Protein-Based COVID-19 Vaccines.” Annual Review of Medicine 73: 55–64. https://doi.org/10.1146/ANNUREV-MED-042420-113212.PubMedGoogle ScholarHotez P. J., Bottazzi M. E., Strych U. 2016. “New Vaccines for the World’s Poorest People.” Annual Review of Medicine 67: 405–417. https://doi.org/10.1146/ANNUREV-MED-051214-024241.GO TO REFERENCEPubMedGoogle ScholarHotez P. J., Kassem M. 2016. “Egypt: Its Artists, Intellectuals, and Neglected Tropical Diseases.” PLOS Neglected Tropical Diseases 10 (12): e0005072. https://doi.org/10.1371/JOURNAL.PNTD.0005072.GO TO REFERENCEGoogle ScholarHotez P. J., Nuzhath T., Colwell B. 2020. “Combating Vaccine Hesitancy and Other 21st Century Social Determinants in the Global Fight Against Measles.” Current Opinion in Virology 41: 1–7. https://doi.org/10.1016/J.COVIRO.2020.01.001.PubMedGoogle ScholarJaggaiahgari S., Munigela A., Mitnala S., Gujjarlapudi D., Simhadri V., Nageshwar Reddy D. 2022. “Heterologous Booster Dose with CORBEVAX Following Primary Vaccination with COVISHIELD Enhances Protection Against SARS-CoV-2.” Vaccines 10 (12): 2146. https://doi.org/10.3390/VACCINES10122146.GO TO REFERENCEGoogle ScholarKim J. H., Hotez P. J., Batista C., Ergonul O., Figueroa J. P., Gilbert S., Gursel M., M.et al. 2021. “Operation Warp Speed: Implications for Global Vaccine Security.” The Lancet Global Health 9 (7): e1017–e1021. https://doi.org/10.1016/S2214-109X(21)00140-6.GO TO REFERENCEGoogle ScholarLalani H. S., Nagar S., Sarpatwari A., Barenie R. E., Avorn J., Rome B. N., Kesselheim A. S. 2023. “US public Investment in Development of mRNA Covid-19 Vaccines: Retrospective Cohort Study.” BMJ (Clinical Research Ed.) 380: e073747. https://doi.org/10.1136/BMJ-2022-073747.PubMedGoogle ScholarLo N. C., Hotez P. J. 2017. “Public Health and Economic Consequences of Vaccine Hesitancy for Measles in the United States.” JAMA Pediatrics 171 (9): 887–892. https://doi.org/10.1001/JAMAPEDIATRICS.2017.1695.GO TO REFERENCEPubMedGoogle ScholarNyon M. P., Du L., Tseng C. T. K., Seid C. A., Pollet J., Naceanceno K. S., Agrawal A., A.et al. 2018. “Engineering a Stable CHO Cell Line for the Expression of a MERS-Coronavirus Vaccine Antigen.” Vaccine 36 (14): 1853–1862. https://doi.org/10.1016/J.VACCINE.2018.02.065.GO TO REFERENCEPubMedGoogle ScholarPino M., Abid T., Ribeiro S. P., Edara V. V., Floyd K., Smith J. C., Latif M. B., G.et al. 2021. “A Yeast-Expressed RBD-based SARS-CoV-2 Vaccine Formulated with 3M-052-Alum Adjuvant Promotes Protective Efficacy in Non-Human Primates.” Science Immunology 6 (61), https://doi.org/10.1126/SCIIMMUNOL.ABH3634.GO TO REFERENCEPubMedGoogle ScholarPollet J., Chen W. H., Versteeg L., Keegan B., Zhan B., Wei J., Liu Z., J.et al. 2021. “SARS-CoV-2 RBD219-N1C1: A Yeast-Expressed SARS-CoV-2 Recombinant Receptor-Binding Domain Candidate Vaccine Stimulates Virus Neutralizing Antibodies and T-Cell Immunity in Mice.” Human Vaccines and Immunotherapeutics 17 (8): 2356–2366.GO TO REFERENCECrossrefPubMedGoogle ScholarPollet J., Strych U., Chen W.-H., Versteeg L., Keegan B., Zhan B., Wei J., Z.et al. 2022. “Receptor-binding Domain Recombinant Protein on Alum-CpG Induces Broad Protection Against SARS-CoV-2 Variants of Concern.” BioRxiv: The Preprint Server for Biology, https://doi.org/10.1101/2021.07.06.451353.GO TO REFERENCEPubMedGoogle ScholarSachs J. D., Karim S. S. A., Aknin L., Allen J., Brosbøl K., Colombo F., Barron G. C., M. F.et al. 2022. “The Lancet Commission on Lessons for the Future from the COVID-19 Pandemic.” The Lancet 400 (10359): 1224–1280. https://doi.org/10.1016/S0140-6736(22)01585-9/ATTACHMENT/959F7B0E-F2C1-4D35-8541-731A847502DC/MMC1.PDF.CrossrefPubMedGoogle ScholarŠuleková M., Fitzgerald K. T. 2019. “Can the Thought of Teilhard de Chardin Carry Us Past Current Contentious Discussions of Gene Editing Technologies?” Cambridge Quarterly of Healthcare Ethics 28 (1): 62–75. https://doi.org/10.1017/S0963180118000397.GO TO REFERENCEPubMedGoogle ScholarTeilhard de Chardin P. 2008. The Phenomenon of Man. Harper Perennial Modern Thought, First Harper Perennial Modern Thought Edition, https://www.holybooks.com/wp-content/uploads/Phenomenon-of-Man-by-Pierre-Teilhard-de-Chardin.pdf (2008).Google ScholarThuluva S., Paradkar V., Gunneri S. R., Yerroju V., Mogulla R. R., Suneetha P. V., Turaga K., M.et al. 2022a. “Safety, Tolerability and Immunogenicity of Biological E’s CORBEVAXTM Vaccine in Children and Adolescents: A Prospective, Randomised, Double-Blind, Placebo Controlled, Phase-2/3 Study.” Vaccine 40 (49): 7130–7140. https://doi.org/10.1016/J.VACCINE.2022.10.045.GO TO REFERENCEPubMedGoogle ScholarThuluva S., Paradkar V., Gunneri S. R., Yerroju V., Mogulla R., Turaga K., Kyasani M., S. K.et al. 2022b. “Evaluation of Safety and Immunogenicity of Receptor-Binding Domain-Based COVID-19 Vaccine (Corbevax) to Select the Optimum Formulation in Open-Label, Multicentre, and Randomised Phase-1/2 and Phase-2 Clinical Trials.” EBioMedicine 83, https://doi.org/10.1016/J.EBIOM.2022.104217.GO TO REFERENCEPubMedGoogle ScholarWorld Health Organization. 2023. “Global Partners Announce a New Effort – “The Big Catch-Up” – to Vaccinate Millions of Children and Restore Immunization Progress Lost During the Pandemic.” https://www.who.int/news/item/24-04-2023-global-partners-announce-a-new-effort-the-big-catch-up-to-vaccinate-millions-of-children-and-restore-immunization-progress-lost-during-the-pandemicGO TO REFERENCEGoogle Scholar
Biographies
Peter J. Hotez, MD, PhD, FAAP, FASTMH is Pediatrician-Scientist and Professor of Pediatrics and Molecular Virology and Microbiology at Baylor College of Medicine where he is also the Dean of the National School of Tropical Medicine and Texas Children’s Hospital Endowed Chair in Tropical Pediatrics. He is also co-director of the Texas Children’s Hospital Center for Vaccine Development. Prof. Hotez has devoted his life to the development of new vaccines for neglected diseases of poverty, including vaccines for human hookworm infection and schistosomiasis in clinical trials, and a new Chagas disease vaccine. During the pandemic he co-led the development of a low-cost and patent free Covid vaccine technology that led to the production and delivery of 100 million doses Corbevax and IndoVac in India and Indonesia, respectively. This provided proof-of-concept that it’s possible to develop and deliver low-cost vaccines at scale bypassing multinational pharma companies. For this work he was co-nominated for the Nobel Peace Prize in 2022. In addition, Prof. Hotez leads efforts to combat rising antivaccine activism in his role as both vaccine scientist and parent of an adult daughter with autism. He is the author of five single authored books including “Vaccines Did Not Cause Rachel’s Autism,” “Preventing the Next Pandemic,” and the forthcoming “Deadly of Anti-Science” each published by Johns Hopkins University Press. He is also the author on more than 690 scientific publications indexed on PubMed, and an elected member of the National Academy of Medicine and American Academy of Arts and Sciences. He was recognized by the AMA with their Scientific Achievement Award and the AAAS with their Scientific Freedom and Responsibility Award, in addition to recognition by the AAMC, ASTMH, ADL, Holocaust Museum Houston, among many others. Prof. Hotez obtained his MD-PhD at Weill Cornell Medical College and Rockefeller University, residency and fellowship training at Mass General Hospital and Yale Univ School of Medicine, and he holds honorary doctoral (DSc) degrees from CUNY, Roanoke College, and Elmezzi Graduate School of Molecular Medicine of Northwell Health. During the pandemic he appeared regularly on CNN, MSNBC, BBC, NPR, PBS NewsHour and other networks communicating to the nation and was recognized for this by the American Medical Writers Association and other organizations.