By Charles C. CamosyOct 16, 2021|

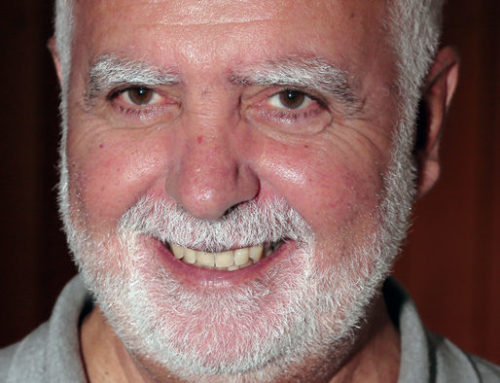
[Editor’s Note: Dr. E. Wesley Ely, MD, MPH is a professor of medicine at Vanderbilt University School of Medicine and the Associate Director for Research for the VA Tennessee Valley Geriatric Research and Education Clinical Center (GRECC). He is also the co-director of the Center for Critical Illness, Brain Dysfunction, and Survivorship (CIBS) Center. Dr. Ely’s research has focused on improving the care and outcomes of critically ill patients with ICU-acquired brain disease He spoke to Charles Camosy about his new book Every Deep-Drawn Breath: A Critical Care Doctor on Healing, Recovery, and Transforming Medicine in the ICU.]
Camosy: Before we get into your book and your specialty in medicine–can you tell us about your philosophy or theology of health care more generally? And about your call to this line of work? I understand that you have been deeply influenced by the Jesuits and take a silent retreat every year? How has this background led to where you are today?
Ely: I was taught by Jesuits and my mom used to be the English Lit teacher at Jesuit Shreveport LA as well. I live by the Ignatian motto, Ad Majorem Dei Gloriam – AMDG – “for the greater glory of God.” As such, I don’t consider this my book. I replace the “my” pronoun with “your” when in prayer about this project because it is not mine at all. I’m just a pencil. Think of Screwtape Letter XIV, and you’ll know my mindset.
You told me about a uniquely Catholic experience you had during COVID. Could you share it with Crux readers and explain a bit about how it informs your own spiritual approach to care with critically ill patients?

As a Catholic, my desire is to meet people where they are. I take patients’ spiritual history and try to respect their pathway to God, as they know Him. If my patient is an atheist, I respect that, of course, and there is a patient story in Every Deep-Drawn Breath (EDDB) on p. 228 about exactly this. An example of a uniquely Catholic experience I had was when I was the physician for a Catholic cardiothoracic surgeon with COVID-19 who was dying from lung failure and blood clots. I went to Mass one morning and brought him the Eucharist. He was so overjoyed at this that I had to remind him to breathe. People have told me that this portion of EDDB is very moving. I’m glad I was able to share such a powerful moment in his life with readers because it speaks to how important spirituality is in medicine and healing, especially when cure is not possible.
Now, onto your wonderful book which tells the story of some of the totally groundbreaking research you’ve done about improving outcomes in the intensive care unit or ICU. During the pandemic we’ve had more opportunities than usual to be aware of what simply being in the ICU does to many patients. I understand it is now recognized as PICS or post-intensive care syndrome? What is PICS?
PICS is the syndrome of diseases that develop mainly in the brain, nerves, and muscles of a person’s body when she or he is critically ill in an ICU. One of the predominant diseases these patients acquire is a rapid onset form of dementia, clinically similar to Alzheimer’s Disease, that ranges from mild to severe and which can last years. About a third of them develop depression, and about one in five suffer PTSD (post traumatic distress disease). The muscle and nerve disease creates a disabling form of physical limitation. PICS leads people to end up retiring early with limitations on their quality of life. The intent of EDDB is to raise awareness of the hope of improvement with the right post-ICU rehabilitation programs.
But you’ve found caring for ICU patients in the fullness of who they are can dramatically improve outcomes, right? Even things like making sure to touch the patient and to attend to their families makes a significant difference? Please say more about what you’ve found.
We have developed a system of medically proven safety steps that we formulated into a bundle called the ABCDEFs or A2F Bundle for short. When used at the bedside, this bundle allows the person to be awake, liberated from life support much earlier, and to engage with loved ones more meaningfully. Overall, this is a program that uplifts the patient and respects each person’s inherent dignity. It’s all about eye contact and respecting the full personhood of each patient and the entire family. While that may sound warm and fuzzy to some who are thinking of the technologically driven environment of the ICU, I assure you, our data are robust and published in the highest tier medical journals, while, at the same time, based on core element of humanity.
This is a remarkable finding on your part, but perhaps just as remarkable is that it hasn’t been discovered sooner – especially because so much of this seems just like common sense when it comes to caring for patients as in the fullness of who they are. I have my own views on why this is likely the case, as anyone who has read Losing Our Dignity knows, but I’m curious about your view. Why was this missed for so long?
Your book, Losing Our Dignity, is a great example of the thought process that drives me each day, Dr. Camosy. I think that one of the reasons it took so long to find our way back to the essence of our calling, to serve others completely, is that medical advances and the beeps and buzzers are very alluring. I was at first drawn to the shiny science and it took my eyes off the person in the hospital gown. I had shame and felt convicted for years, which drove me to get the funding to do these studies to disprove the status quo in lieu of this newer way with the A2F Bundle. It feels good to be back on track, especially when for many years afterwards, I’m in contact with survivors of the families of the deceased who tell me how powerful their ICU experience and recovery period were for them. I think about the line from the Serenity Prayer, “Accepting hardship as a pathway to peace.” Whatever I can do to reduce human suffering is good, and if that hardship in their lives can ultimately become a pathway to peace, then it was my privilege to be a widget along the way.
So much of what you have found and stand for as researcher and clinical either comes out of or is consistent with doing medicine in a theological context. But obviously there are challenges in today’s environment for doing that. How can we reconnect theology to medicine in our contemporary context?
I believe it all boils down to our purpose. I am not there for me, for career success, money, or fame. Nightly, because I have a problem with pride, I say the Humility Novena with my wife. I am there to allow God to insert me into other’s lives to provide mercy. I want to dive into the chaos of their lives and provide lifting and healing. Mercy. If that isn’t connecting theology to medicine, then what is?
Catholic doctor seeks to help patients better recover from ICU | Crux Now